Laurie's Blogs.
Aug 2018
Balancing Evidence Based Practice & Clinical Practice
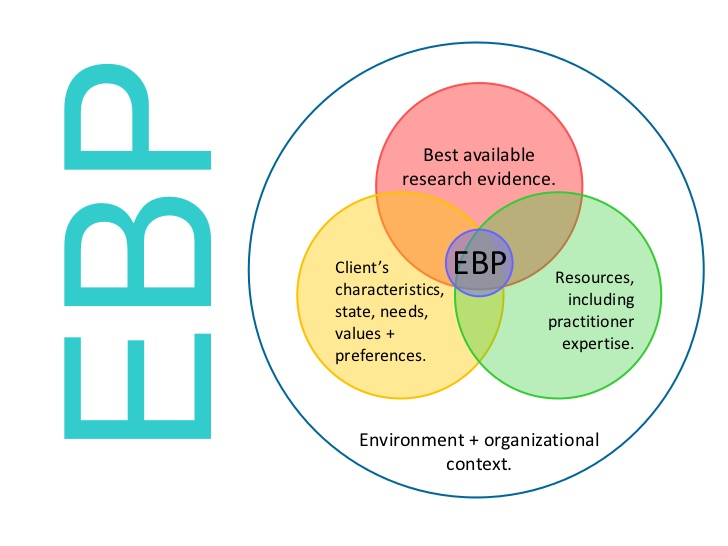
How do you find balance? How do you justify what you do? How do you forge ahead and make discoveries? You might think this is a ‘lifestyle’ blog. Not so! This blog is about finding balance between ‘clinical practice’ and ‘evidence based medicine’, and how you balance those two for the benefit of your patients and to defend or justify your choices. If all you chose to do was ‘evidence based’… you’d have a much shorter list of what you utilize and prescribe, and HOW you use the therapies you use would also be abbreviated.
Now, don’t get me wrong. I love research, and if you’ve ever been to one of my lectures, workshops, or even read one of the Four Leg Newsletters, you’ll see that I LOVE referencing! I love finding research and I love justifying my opinions and practices. For example, I know I’ve heard (and I bet you have as well) … “Show me the research that this ‘Canine Rehab’ stuff works on animals!” I think, are you kidding??!! Everything we know about the individual treatments HAS been validated on animals. ALL modalities have been studied on animals first before being applied to humans (thank you rats!), and now we’re just using them to TREAT the animals (instead of just testing on them). What we know about the neurophysiological effects of mobilization & manipulation – again, rats! Exercise physiology? Humans, dogs, horses… and of course, rats! The trouble is that you have to search through mountains of individual research papers and search key words as they pertain to specific treatment tools and techniques to find what you need to justify therapeutic choices. (i.e. shockwave tendon). If you search ‘canine rehabilitation tendon’, you might not get much at all! So, you need to search everything you might potentially include in a CLINICAL rehab program in order to find justification for what you do. What if you don’t KNOW what to include in a clinical rehab program? Well then, I guess you have to ‘guess’ when you’re online to do your Pubmed search, and read through dozens of abstracts! Some of those abstracts might lead you to other ideas / suggestions in regards to treatment. (P.S. Here’s the link to Pubmed: https://www.ncbi.nlm.nih.gov/pubmed )
You can’t just rely on what you were taught in class. Things change and evolve. How would you make decisions when it comes to new technology or when confronted with an unusual case? This makes me think about a recent communication with a Vet Board up here in Canada. They wanted to see some kind of evidence that physiotherapists have training and education in the application of modalities to animals. I was a bit flabbergast. What profession has MORE background in modality application, regardless of the species? But, because I was tasked with having to prove this, it led me to search through the wording of the human physiotherapy regulatory boards to see how they deal with the regulation of modalities and ‘new or emerging’ modalities. For example, I didn’t learn about microcurrent or shockwave in my physiotherapy degree. Those technologies weren’t clinically utilized at the time. I don’t even know if they existed at all! However, both are currently utilized in human physiotherapy practice now. So, what does the regulatory language have to say about such things?
A footnote in the Entry-to-Practice Physiotherapy Curriculum: Content Guidelines for Canadian University Programs (May 2009) states that, “Decisions by individual academic programs regarding which modalities to include in their curriculum will be based on the available evidence. As the evidence changes, this list will evolve.”
The College of Physiotherapists of Ontario offers the following tool to assist PTs in making decisions about whether or not they should use a particular modality/treatment, https://www.collegept.org/rules-and-resources/is-it-physiotherapy. In addition, Physiotherapists must follow the standards of practice associated with the safety and maintenance of the modality as outlined in section 3 of the Infection Control and Equipment Maintenance Standard, https://www.collegept.org/rules-and-resources/infection-control-equipment-maintenance. It remains the responsibility of the physiotherapist to be trained and knowledgeable on the safety of modality tool and its application. Resources to learn about safety of specific equipment can be found through the Health Canada website and by through the vendor directly. The College also recommends that the physiotherapist discuss the proposed treatment and use of the emerging modality and the evidence with the patient to inform the patient’s decision and choice to proceed with the treatment or not.
Okay, so in the context of clinical practice. CLINICAL innovations in uses of any modality, exercise principle, manual therapies, or novel therapeutics will always come from CLINICAL practice first! Look at massage. Nobody did research on that first before people began applying it, liking it, and finding it to be beneficial! Different weight training regimens… those are tried and tested in a gym. If someone has success, they tell others… and on down the line some researcher puts the concept(s) into a study. But new CONCEPTS are developed in clinical practice. Use all of that science background and put it to good use… if you are looking at using a new modality, learn what it does, learn about its effects on physiology, and you decide, test, and trial how you will apply it. The same goes for exercises – test them, look at how a patient does them, evaluate effectiveness, and re-utilize if appropriate or revamp if you don’t get the desired effect.
The application of ‘physical therapies’ requires a professional approach: 1) evaluate the situation and what you want to achieve, 2) evaluate the tools at your disposal to select the best ones possible, 3) Decide the optimum dosing (per session, per day / week / month) based on the ‘Best Available Evidence’, 4) Try new things, innovate, experiment, and create. I believe that the latter is the responsibility of clinicians. Clinical practice is what generates new ideas, techniques, and protocols. If everyone were to treat using ‘a cookbook’, the profession (any profession) would stagnate!
So, go out there this week, try something different. Search the literature… see if there is anywhere that might justify you ‘tweaking’ your current protocols. If an animal isn’t responding like you’d want or they are not progressing quickly enough, try something new! Challenge the status quo! Much of what I’ve learned along the way has been trial and error, justified or explained after-the-fact with pieces of research. Don’t be afraid to step outside of the box!
Have a great week folks! (And let me know if you discover something new!)
Cheers! Laurie